CURES ACT LEGALIZES DEFINED CONTRIBUTION FOR INDIVIDUAL PLANS
Today, President Obama signs the 21st Century Cures Act into law and in doing so legalizes “qualified small employer Health Reimbursement Arrangements” (QSEHRAs). This provision, tacked on at the end of the law, is by no means the most important piece of this legislation. The bipartisan agreement, which has been heavily praised by the White House, does a lot of good things if you ask most lawmakers but doesn’t go far enough for Bernie Sanders, Elizabeth Warren, and a few others. A bill that was strongly supported by Vice President Joe Biden, the Cures Act will transform cancer research and accelerate discoveries. It also funds the fight against the opioid epidemic, invests in research on brain diseases like Alzheimer’s, and addresses mental health issues with bipartisan policies. It’s one of President Obama’s last big victories while in office, and, collectively, our elected officials are patting themselves on the back for this one, as they should. If you’re not yet familiar with the new law, you should take a few minutes to read about it.
For the health insurance industry, the Qualified Small Employer HRA provision is also a big deal, though it’s not yet on most people’s radars. As of today, Tuesday, December 13, 2016, defined contribution for individual plans is finally legal. This is a battle we’ve been fighting in the insurance industry for at least the last decade, and with the stroke of a pen President Obama says it’s perfectly fine for a small employer to pay for individual health insurance for its workers. This is something the administration has publicly opposed in the past, but he was willing to compromise in order to get the bill passed.
Over the years, I’ve written countless presentations, CE classes, white papers, and articles about defined contribution. My position, like many in the industry, has always been that defined contribution isn’t yet legal but that it probably should be. I’ve also worried about the possible impact on the small group market, though I’m not as concerned as some people are. As we move forward, I’m sure I’ll have some thoughts about how brokers can use this new law to help their clients and grow their business. For now, though, I want to focus on what’s in the “other provisions” section of the Cures Act.
SEC. 18001. EXCEPTION FROM GROUP HEALTH PLAN REQUIREMENTS FOR QUALIFIED SMALL EMPLOYER HEALTH REIMBURSEMENT ARRANGEMENTS.
In Title XVIII, Section 18001 of the 21st Century Cures Act, we find the language related to defined contribution. It totals 2,380 words, many of them identical to the language in the Small Business Healthcare Relief Act, a previous bill that had bipartisan support in both chambers of Congress and the endorsement of the U.S. Chamber of Commerce, the National Association of Home Builders (NAHB), the National Federation of Independent Business (NFIB), the American Farm Bureau Federation (AFBF), and several other organizations.
The provision modifies the U.S. Internal Revenue Code to create an “Exception for Qualified Small Employer Health Reimbursement Arrangements,” exempting them from the requirements applicable to group health plans. A QSEHRA is defined in the law as an arrangement “funded solely by an eligible employer” with “no salary reduction contributions” permitted. In other words, employers can put money in an HRA for employees to use, but employees cannot add their own pre-tax dollars through a section 125 plan.
The reimbursement is only available after an employee provides proof that he or she (or a family member) incurred an expense for medical care as described in section 213(d) of the tax code—including the premium paid for an individual health insurance policy. Employers can contribute up to $4,950 for single coverage and $10,000 for family coverage, indexed for inflation.
Obviously, there are a lot of additional details about what is and is not allowed. Here are the high points:
- The employer can vary the contribution based on variations in premium that are attributable to age or the number of family members covered. The variation would be “determined by reference to the same insurance policy with respect to all eligible employees.” In other words, the employer would pick a reference plan, much like the current process in the SHOP exchange.
- The HRA contribution should be prorated based on the number of months that the employee is covered.
- Eligible employees can participate in the HRA. The employer can apply a 90 day waiting period and can exclude part-timers from eligibility.
- Only non-applicable large employers (small employers not subject to the employer mandate) who do not offer a group health plan to their employees are allowed to offer a Qualified Small Employer Health Reimbursement Arrangement.
- Employers offering a QSEHRA must provide a notice to employees at least 90 days before the beginning of the plan year 1) indicating the amount of the reimbursement, 2) telling employees that they must notify the exchange about the reimbursement if they are applying for a premium tax credit, and 3) letting them know that they are still subject to the individual mandate and that the reimbursement will be treated as taxable income for any month in which they do not have minimum essential coverage. Failure to provide the notice will result in a fine of $50 per employee up to a maximum of $2,500.
- Reimbursements under a QSEHRA are excludable from gross income if the employee has minimum essential coverage.
- The reimbursement under a QSEHRA will disqualify employees and their family members from receiving a premium tax credit if the remaining amount they would have to pay (after receiving the HRA reimbursement) for single coverage for the second-lowest-priced silver-level plan in the federal or state marketplace would be less than 9.5% of their household income (indexed for inflation after 2014). In other words, the family glitch is built into this new law.
- Employers subject to the ACA’s W-2 reporting requirements must report the amount available through a QSEHRA on the employees’ W-2s. (This shouldn’t have an immediate impact since employers with fewer than 50 FTEs can offer a QSEHRA but currently only companies issuing 250 or more W-2s are subject to the reporting requirement.)
- Qualified Small Employer HRAs may be offered as early as January 1, 2017, but there is transition relief exempting any company already offering such an arrangement from penalties under section 4980D of the tax code. The IRS has threatened employers with a $100 per day per employee penalty in the past.
- Qualified Small Employer HRAs are not subject to COBRA continuation requirements.
Impact on the Industry
Again, I’ll hold off on talking about the opportunity this creates for insurance agents and their clients. The fact is that whether this is truly an opportunity will depend on the strength of the individual market, and right now it’s a mess. Don’t expect a lot of employers to drop their group plans and send their employees to the individual market, not right away at least. However, if the ACA replacement plan is successful at bringing down costs in the individual market, defined contribution could become a viable strategy.
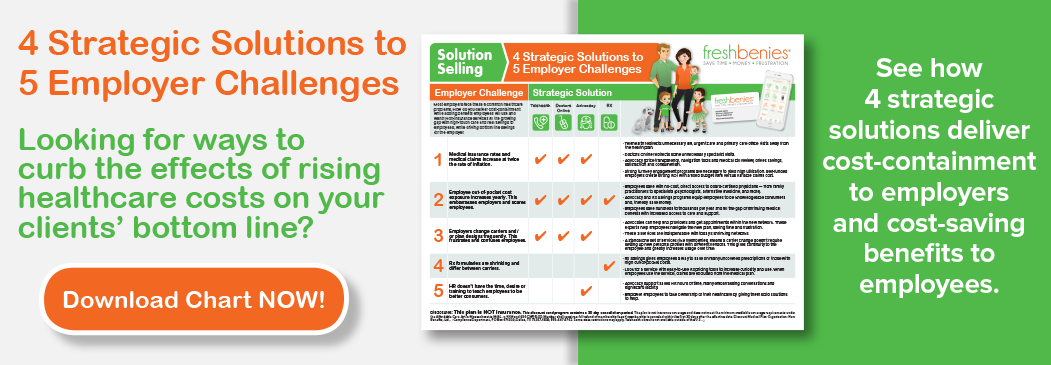
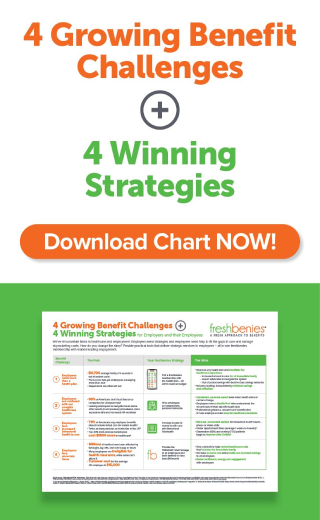
Either way, one trend we’ve witnessed is likely to continue: today’s health plans do not provide comprehensive coverage, so additional products are needed to fill the gaps, including supplemental insurance, telehealth, prescription savings programs, and more. These benefits, whether sold on a group or individual basis, should be offered alongside the health plan as part of a total solution, not mentioned as an afterthought at the end of the conversation.
In closing, we already knew 2017 was going to be a crazy year. With defined contribution now legal for qualified small employers, it just got a little crazier.
Now it’s your turn! How do you think this change in defined contribution will affect the insurance market? What part of the Cures Act do you see as most impactful? Comment below or email me at eric@freshbenies.com.