TODAY’S EMPLOYEE BENEFIT PLANS: 3 REASONS UTILIZATION IS CRITICAL
How do you gauge success of the benefit plans you sell to your groups? Maybe it’s staying within your client’s budget, keeping coverage for spouses and families, and ticking off boxes of the “must-haves.”
Those things absolutely matter. But, in today’s consumer-driven health care system, utilization is an important piece of the puzzle in the success of a total benefits package. Utilization reflects the group’s satisfaction, improves their ROI, and increases retention year after year. These results all strengthen loyalty and reflect on you as the trusted consultant.
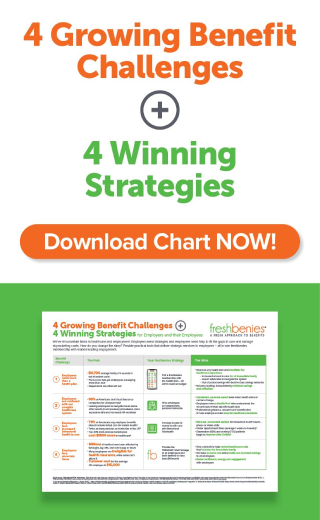
I’m sharing 3 points on how utilization is critical to ROI.
1. High utilization is the new math
In the insurance space, you typically want low utilization, right? But the inclusion of non-insurance services within the total benefits package turns that thinking around. When an employee uses telehealth instead of an in-office, urgent care or ER visit, it keeps costs from hitting the employer health plan (while improving the out-of-pocket expense and convenience factors for the employee). High use of certain services go up, and costs stemming from other types of care go down. So, it’s easy to see why a strategy to drive high utilization makes sense. But it does take a strategy…
2. “Included” doesn’t equal usage
The most common concern I address daily is, “Why pay for something that’s included in the medical plan?” On the surface, this question makes sense. However, looking at usage will quickly bring the idea of utilization into play.
For example, the average usage of carrier-installed telehealth is 2%. Imagine a group of 100 employees having only 2 consults for the entire year. That won’t deliver savings (to the employer or the employees). What if we look at industry-wide telehealth utilization? Not a huge difference, the average is still just 7%. So why aren’t employees using it?
They are! At freshbenies, we see an average telehealth utilization of 58% (and 90% when employers follow our 3 best practices). That same example of 100 employees would have 58 consults a year. When each visit can save hundreds of dollars, the savings from that kind of use delivers a real ROI.
Once you realize the employee engagement is very low with an “included” carrier-plan, you quickly realize high utilization is infinitely more valuable than a lower monthly cost.
3. Delivery drives utilization (and savings!)
The difference between 2% and 58% utilization comes down to delivery. If you want a winning strategy to drive use of consumerism tools like advocacy, telehealth and online specialty consults, you must evaluate how services are delivered to the employees.
• What turnkey communications are in place to drive awareness?
• How is the member experience? (i.e. Is there an additional cost to use the services? What technology is available to use the service? Is the family included in a membership?)
• What kind of support is in place to support the employer? (i.e. Can they monitor utilization throughout the year? Is there an expert available to help employers foster usage?)
There are some great options available that truly drive utilization, so you don’t have to rely on an inefficient solution just to quickly tick the box of offering a benefit. Wouldn’t you rather advise your groups on the best strategy and have the employer and employees “utilize” you for years to come?
Now it’s your turn! How have you been evaluating utilization with your clients? How do you approach use of consumerism tools in the total benefits plan? Comment below or email us at brokers@freshbenies.com.