The Five C's of Insurance Sales
We all learned about the 3 Rs in grade school (two of which, ironically, don’t begin with the letter R). And those of us who took business classes in college learned about the 4 Ps of marketing (product, place, price, promotion). In this article, I’ll introduce a new success strategy for agents and brokers: the 5 Cs of insurance sales.
From my experience, I believe that insurance advisors must do a bare minimum in each of these areas if they want to be taken seriously, but those who focus on just one or two and become really good at them can enjoy incredible sales success.
The Five Cs
I’ll start off by discussing each of the five Cs, then I’ll suggest a strategy that will help you stand apart from the competition.
COST
Insurance premiums are skyrocketing and our clients have limited budgets, so cost is not something that can be ignored. And really, when we discuss cost we need to look at both premiums and penalties since both have an impact on the employer’s bottom line and your success with insurance sales.
This is an area that agents have spent a considerable amount of time on over the past few years. With the rollout of the Affordable Care Act and the employer shared responsibility requirement, cost is a big issue for employers and it needs to be a priority for agents as well. That said, it is possible that agents have focused a little too much on cost. Here’s why.
When you make cost containment your number one priority as an insurance agent, you’re left with three pretty big problems:
1) First, clients are never going to be happy with the cost of health insurance, so if this is what you use to differentiate yourself, you’ll continually fall short of your clients’ expectations. They’ll always be unhappy and will always be looking for a better deal because you yourself have convinced them that price is the most important factor.
2) Second, there’s not much you can do about the price of health insurance. Sure, you can suggest cost strategies like increasing the OOP, reducing the provider network, and tweaking the formulary, but once those changes are made, the rates are the rates. There’s very little you can truly do that another agent can’t also do. Still, cost is important, so you better understand all the cost-containment strategies and know which ones are right for which clients—just don’t make it your sole priority.
3) Third, and most importantly, agents who focus so intently on cost strategies for insurance sales tend to do so to the exclusion of the other four Cs, and that’s a problem because, as I’ve already said, you must do a bare minimum of each of these if you want to hang on to your current clients and win some new ones. You don’t have to excel in every area, but there is a minimum threshold that must be met.
COMPLIANCE
The funny thing about compliance is that it’s also a cost strategy. That’s because the penalties for compliance failures are often bigger than the employer mandate penalties under the health reform law, and since the risk exposure created when a company offers employee benefits is so significant, it has to be factored into the employer’s decision. There’s also a cost associated with the time it takes to stay compliant. HR managers spend countless hours—all of which could be better spent on other tasks—trying first to figure out and then to follow all the IRS and DOL rules and regulations.
In addition to cost, though, there’s also a hassle factor to offering benefits, and agents who can help their clients stay compliant and avoid penalties while making the entire process a little less painful will be in high demand. It’s sort of like going to the dentist—yes, it costs money, but that’s not the main reason so many people dread it. They’re scared it’s going to hurt. If your clients are complaining about all the new reporting requirements, just give them something to numb the pain. You don’t need to offer them a free solution like Zenefits is doing, but you do need to have a solution.
CONSUMERISM
For the past 15 years now, the insurance industry has been obsessed with the concept of consumerism. Give consumers some skin in the game and the tools they need to be wiser health care consumers, the theory goes, and they’ll buy health care the same way they do everything else. As a result, quality will go up and price will go down. Just look at Lasik surgery, blah, blah, blah…
Agents have certainly talked a good game, but now it’s time to deliver. Consumerism isn’t going away. The plan design changes that usually accompany a consumer-directed approach are happening regardless of whether we try to build better health care consumers are not – they’re part of the cost strategy we’ve already discussed. Deductibles and out-of-pockets are going up, copays are going away, drugs are being moved to non-formulary. People need to become better health care consumers because today’s plan designs require it.
This is not an intuitive process, though, and if we’re going to sell the plan design without giving employees the tools they need, they’re not going to figure out how to “shop around” and “negotiate with providers” on their own and, as a result, will end up hating their benefits. And if they hate their plans, why offer health insurance in the first place?
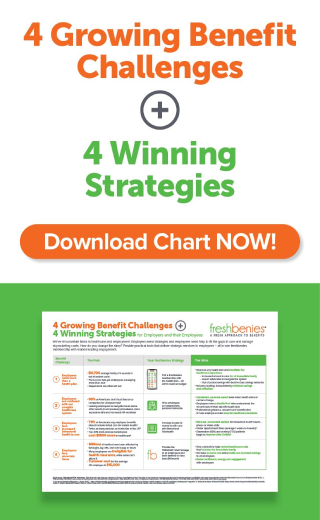
The good news is that there are a lot of tools and non-insurance benefits out there that, to use the previous analogy, can help numb the pain for employees of all of these plan design changes. If you’re going to increase out of pockets, drop copays, and take away doctors, give employees a telehealth benefit so they can still consult with a physician at a reasonable price. If you’re going to drop ancillary benefits, at least give your employees some dental and vision discounts to help keep the costs reasonable. If you’re going to ask people to shop for health coverage, give them some price transparency tools. As a broker, you can’t just take away benefits without filling some of the holes.
CHOICE
If you have to take away benefits to keep costs under control, one way to soften the blow is to let the employees decide to take a lesser plan rather than having the employer make that decision for them. In other words, if the old plan is going up by 30%, instead of replacing it with a lower-cost plan that employees are going to complain about, the group could continue to offer the expensive plan at the new higher price but introduce a new lower-cost option and let employees choose which one they want. When employee choose their health plan, it’s harder for them to blame the employer if they don’t like it. It also helps them understand that there’s a tradeoff between coverage and benefits.
Choice is a big part of consumerism. It’s impossible for people to shop if they don’t have options, and those options begin with the health plans themselves. Even if people choose a low-deductible plan with copayments over a higher deductible HSA-compatible plan, the act of choosing makes them stop and think about how they use their benefits, and that’s a good thing.
The number of options available to people is going to continue to increase, at least until all of the big insurance carriers have merged into one. In the individual market, for instance, Healthcare.gov and the state-based exchanges are offering individuals and families a multitude of options from different insurance companies. For small employers, the SHOP exchange that nobody’s participating in was supposed to do the same thing. For larger employers, the growth of private exchanges will make it much easier to let employees design their own benefit plans.
It is important, though, not to go overboard with all of this choice. Giving people options is definitely a good thing, but when they have too many options employees can have a tough time making a decision, especially when they don’t understand those options (News flash: People don't understand health insurance, so they won't understand their options). It’s important for brokers to limit the number of options they present to employers and offer to employees. Give them enough choice but not too much choice.
It’s also important to note that not everything should be a choice. If a company is offering a benefit that can help the employees save money while reducing the claims that the employer or insurance company will be responsible for, it’s a no-brainer that all employees on the health plan should have that benefit. Instead of making it voluntary, the employer should consider paying for it since the benefit has a positive ROI. Telehealth is a good example. A well-designed wellness program is another. If the employer understands the value of the program but the employees won’t, then it shouldn’t be offered on a voluntary basis; it should be employer-paid.
COMMUNICATION
I once heard an old man say that running a business without a sign is like whistling at a pretty girl in the dark: you know what you’re doing, but nobody else does. I’m not sure exactly what that means, but somehow it seems appropriate to the topic of benefits communication. If a company offers a benefit but doesn’t tell its employees about it, it’s not really a benefit. You have to tell the employees what their options are so they’ll make the decision to sign up for the various types of coverage that are being offered; then you have to make sure they understand those benefits so they’ll use them properly. Otherwise, the company’s just wasting its money.
I’m continually amazed by employers that spend tens or even hundreds of thousands of dollars on employee benefits but can’t spare the time to let the broker do a proper enrollment and orientation meeting. It is your job as a broker to make sure employees understand their benefits. And in order to get in front of the employees, you may need to challenge the employer a little bit. If your client says there’s no time for an employee meeting, you need to explain that it can significantly increase the company’s ROI. If he or she suggests a voluntary enrollment meeting, lobby for a mandatory one. Your job is to make your client look like a hero to the employees, and you can only do that if you actually get to talk to them.
The good news is that most brokers don’t do a good job with benefits communication, so this is an opportunity for you to really set yourself apart from the competition.
The Strategy: do it all, but specialize
As I’ve already said, none of the five Cs is optional—you must do each of them to some degree. It’s expected, and it’s the price of entry for an insurance agent. But once you’ve met the bare minimum, you need to do something to differentiate yourself, to make what you offer different from (and better than) the next guy.
I mentioned Zenefits earlier. They’re a great example of a company that has chosen to focus on one of these five areas: compliance. Zenefits’ HR software saves Human Resource professionals time and frustration and helps ensure their clients are in compliance. That’s definitely a value add.
But instead of crying foul or worrying that Zenefits is going to steal your clients, you should recognize their approach for what it is: a specialization strategy. The way to compete isn’t to go do the exact same thing but rather to do something different. If Zenefits focuses on compliance, why not focus instead on offering a consumer-driven solution that really empowers the employees to make better decisions and arms them with the tools they need to succeed? Or why not spend more time communicating the benefits the employer is paying for so the employees love working for the company? There are a lot of ways to differentiate yourself, to do things better than Zenefits or any other competitor out there. So pick one.
But before deciding to specialize, you need to understand that the compliance problem isn’t going to go away. You need to find a solution for your clients that will “numb the pain” of staying compliant and help them avoid penalties, so find a good third party administrator who can help them out for a reasonable fee. Again, it doesn’t have to be a free solution, but you do need to have a solution. The agents that are most vulnerable to losing AORs to Zenefits or other competitors that focus on compliance are those who’ve given the standard “that’s an employer law, not an insurance law, and my E&O doesn’t cover it” answer to their clients. Don’t do that…
Thanks for reading, and good luck!